Navigating Healthcare’s Future: A SWOT Analysis Part 2: Strengths and Threats!
A Virtual Ward and Remote Monitoring SWOT Analysis: Strengths and Threats (Part 2 of 3)
In the first instalment of this three-part series, we touched on the transformative expectations and circumstances surrounding NHS England’s plans for the deployment of Virtual Wards. Programmes of this scale across an organisation as complex and diverse as the NHS are always challenging. Success requires a common vision, goal, and commitment, none of which can be achieved without collaboration across multiple stakeholders, as well as the funding and time to support the journey to the new models.
Despite the “usual” transformation challenges, such as growing waiting lists, resource shortages, and the impact of strike disruptions—we must keep our eyes on the prize. Virtual Wards and Remote Monitoring represent one of the very few viable and scalable pathways to improve patient welfare. The combination of new clinical practices and technology enablement delivers results, such as preventing unnecessary admissions and identifying deteriorating patients as well as enabling earlier discharge post procedure. While not a panacea for all healthcare woes, these technologies do provide a means to prioritise high-acuity patients and place them at the centre of their healthcare journey.
As we continue to explore the topic, this second post will focus on the Strengths and Threats to Virtual Wards and Remote Monitoring implementation. Drawing from both industry data and firsthand experiences, we’ll examine some of the key strengths that make Virtual Wards and Remote Monitoring a cornerstone for future healthcare delivery, as well as the potential pitfalls that represent a challenge to their full-scale adoption.
💪 Strengths:
1. Evidence-Based Approach
2. Patient-Centric
3. Multidisciplinary Care
4. Resource Optimisation
5. Technology-Enabled. 🚀✨
🌊 Threats:
1. Transformation Challenges
2. Technology Barriers
3. Quality of Care
4. Variable Outcomes🛡️💼
Strengths
1 Evidence-Based Approach
The concept of an “Evidence-Based Approach” in the context of Virtual Wards refers to the utilisation of empirical data, research findings, and case studies to validate the effectiveness and viability of Virtual Wards. This approach is not just theoretical but is backed by practical outcomes that demonstrate benefits for both patients and healthcare systems. The guidelines cite in the supporting notes evidence of benefits including reduced hospital admissions, positive patient feedback, case studies, quantitative safety, and satisfaction metrics, plus broad clinical support.
2 Patient-Centric
The Patient-Centric nature of the Virtual Ward model refers to the model’s focus on delivering healthcare that is tailored to individual patients’ needs and preferences, including allowing, when appropriate, patients to receive medical care in the comfort of their own homes, thereby enhancing their overall healthcare experience. However, patient-centric care goes beyond purely the location and includes personalised care, informed consent and education, improved patient community engagement, plus clear options regarding communications with regard to safety, such as who to contact if their symptoms worsen. For many, these reflect extremely positively when it comes to patient satisfaction, and there are many examples of patients expressing their preference for virtual and remote care versus the alternatives.
3 Multidisciplinary Care
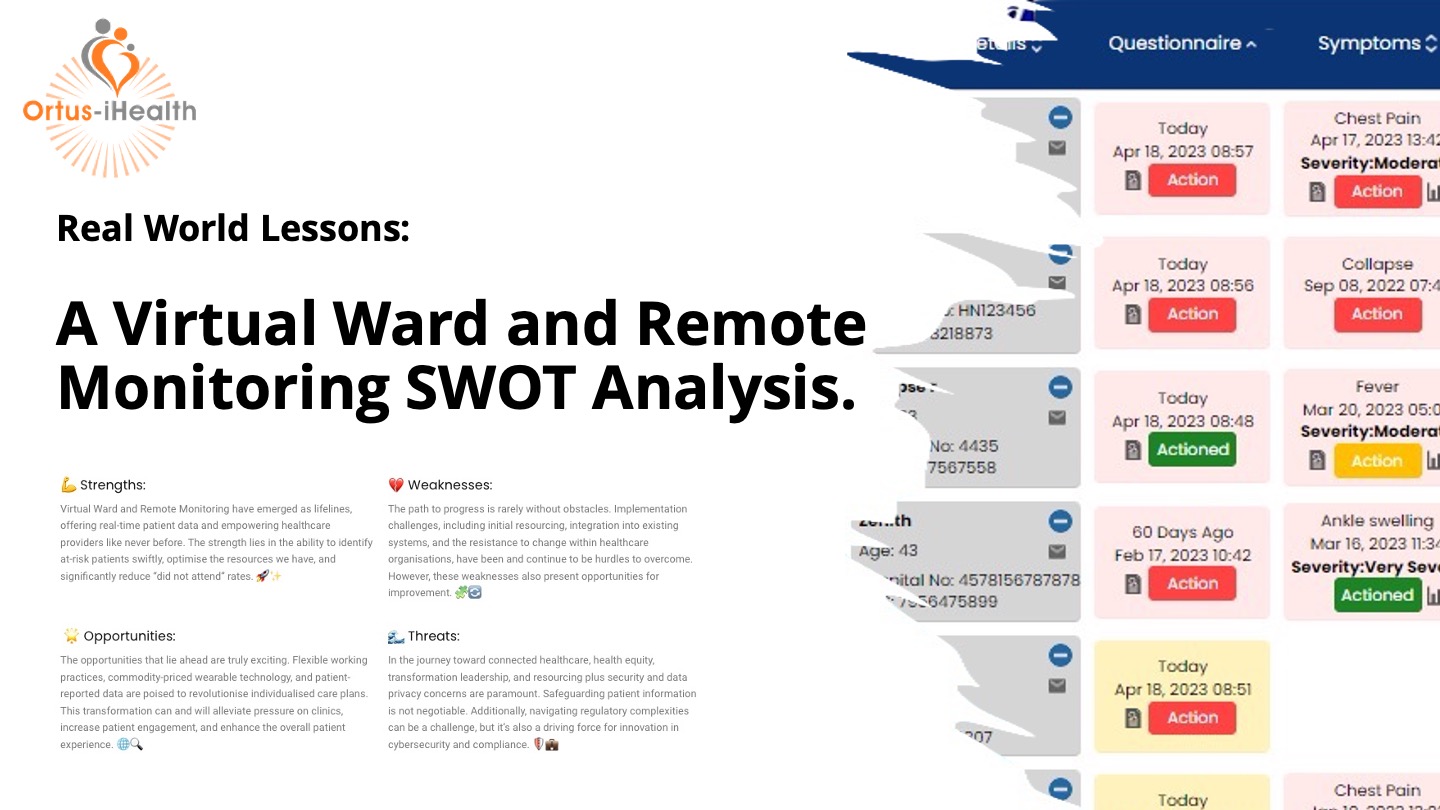
Virtual wards with their active dashboards enable “Multidisciplinary Care,” embracing the ability to deliver a collaborative approach involving a team of healthcare professionals from various disciplines. This team is usually led by a consultant practitioner or Advanced Nurse Practitioner and may include senior consultants, nurses, general practitioners, pharmacists, social workers, and other specialists as needed. With ready access to a wealth of qualified data and managed escalations, the approach can minimise the issue of availability of personnel and expertise, supporting timely interventions and continuity of care across care settings.
4 Resource Optimisation
Virtual Wards contribute significantly to healthcare resource optimisation by effectively reducing the need for additional secondary care beds. A virtual ward of 50 beds could provide the equivalent of 31 extra secondary care beds. They also have a positive impact on reducing emergency department presentations and hospital admissions. Economically, while not the primary focus, Virtual Wards have shown to reduce overall resource use and costs, making them a cost-effective solution. On the workforce front, Virtual Wards allow for more flexibility for the staff. They offer opportunities for flexible working arrangements and blended roles that combine in-person and virtual clinical care. This flexibility enhances staff experience and reduces turnover, indirectly contributing to resource optimisation. The quick and safe implementation of Virtual Wards also adds to their strategic value in resource management.
5 Technology Enablement
The use of MedTech and Software as a Clinical Device in Virtual Wards offers practical benefits. Remote monitoring reduces the need for physical beds, providing a scalable and cost-effective healthcare solution. Real-time data tracking enables timely interventions, preventing unnecessary hospital stays. From a workforce standpoint, technology allows efficient staff use. It supports flexible work arrangements, improving staff experience and reducing turnover. A comparison between tech-enabled and traditional Virtual Wards showed efficiency gains, including shorter stays and better nurse-patient ratios. The investment in technology yielded a significant return, reinforcing its economic viability. Overall, technology in Virtual Wards offers an efficient healthcare approach.
Threats
1 Transformation Challenges
Transformation Challenges pose a significant threat to the effective deployment of Virtual Wards. Implementing a new model of care requires not only technological adjustments but also changes in clinical practices, workflows, and staff training. Resistance to change from healthcare professionals, coupled with the complexities of integrating Virtual Wards into existing healthcare systems, as well as governance and integration needs, can impede the smooth transition and uptake of this innovative model. Additionally, the lack of a unified vision and commitment across stakeholders can further complicate the transformation process, undermining the potential benefits of Virtual Wards.
2 Technology Barriers
Technology Barriers can severely limit the effectiveness of Virtual Wards. While technology is a cornerstone of this healthcare model, issues such as poor internet connectivity, lack of interoperability between different healthcare systems, and digital exclusion among patients can hinder its successful deployment. The maintenance of analogue pathways for patients with specific needs is also required. These barriers can result in unequal access to care, exacerbating existing health inequalities. These areas need further investment and development.
3 Quality of Care
The model aims to provide healthcare that is as effective as traditional in-person care. However, the reliance on remote monitoring and virtual consultations can potentially compromise the quality of clinical assessments. Misdiagnoses, delayed interventions, and lack of hands-on care can result in suboptimal patient outcomes, casting doubts on the efficacy of Virtual Wards.
4 Variable Outcomes
The success of this model is highly dependent on multiple factors such as the complexity of medical conditions being managed, the proficiency of healthcare providers in using the technology, and patient adherence to remote monitoring protocols. Inconsistent results across different settings and patient populations can undermine the credibility of Virtual Wards, making it challenging to secure long-term investment and support for this model.
To Conclude
So to summarise the story so far, we’ve explored the NHS’s ambitious plans for Virtual Wards, noting both their strengths and threats. As we’ve seen, these wards offer scalable, evidence-based healthcare but face hurdles like technology barriers and transformation challenges. Stay tuned for the final instalment, where we’ll delve into Opportunities and Weaknesses.
What are your thoughts on Virtual Ward and Remote Monitoring? What have your experiences been of the vrtual journey so far? Please share your questions and thoughts and let’s engage in a meaningful conversation. Share your insights in the comments below! 👇🤝
Related Posts
Navigating Healthcare’s Future: A SWOT Analysis of Virtual Ward & Remote Monitoring in the UK NHS
A Virtual Ward and Remote Monitoring SWOT Analysis (Part 1 of 3) As professionals in the healthcare industry, we are witnessing a monumental shift in patient care. The adoption of Virtual Ward and Remote Monitoring technology within the UK NHS has been a game-changer. 🇬🇧💡 In my role at Ortus-iHealth, I’ve had the privilege of […]


Leave a Reply